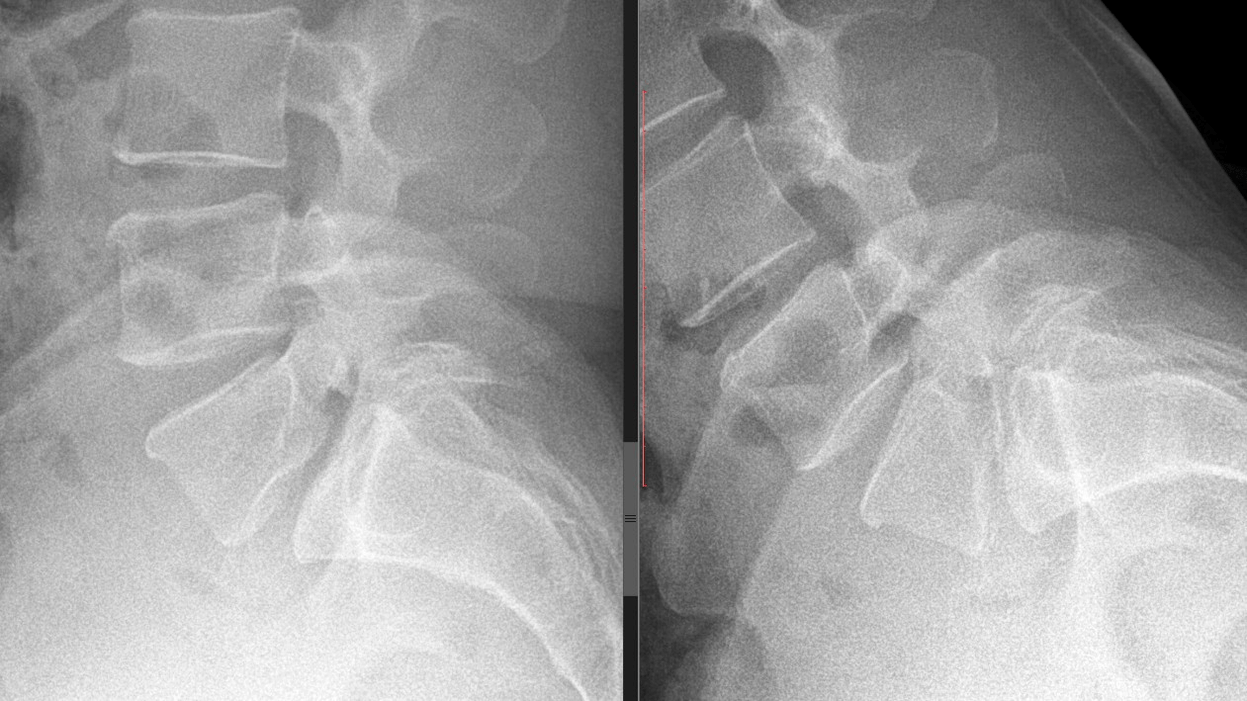
Osteochondrosis is a common pathology of the spine, characterized by a dystrophic change in the structure of the cartilaginous discs of the vertebrae and their bone base. To some extent, osteochondrosis manifests itself in most people after the age of 30. The symptoms of cervical osteochondrosis are varied, which often makes diagnosis and subsequent treatment difficult.
General symptoms and signs of cervical osteochondrosis
The osteochondrosis process affects any part of the spine or several at once. The lumbar and cervical vertebrae are most susceptible to pathology, as they are the most susceptible to stress due to the anatomy of the human skeleton.
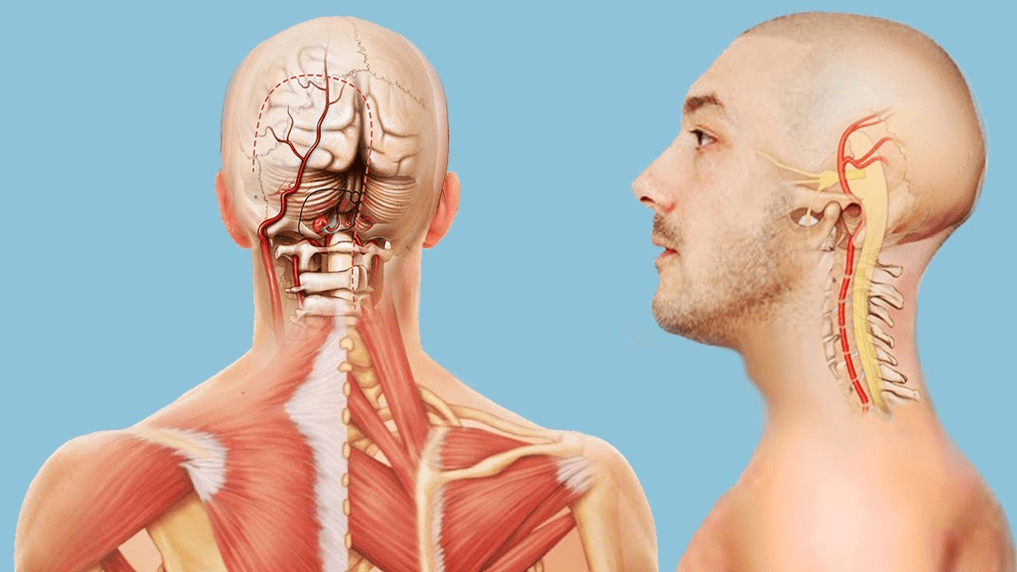
The consequences of osteochondrosis of the spine in the neck region cause the most inconvenience and potential complications, since the neck is an area rich in neurovascular pathways, many of which directly supply the brain. For this reason, the clinical symptoms of cervical osteochondrosis are largely associated with ischemia of brain areas. In addition, the nerve roots, which provide the sensitivity and motor activity of the arms and shoulder girdle, can produce a variety of symptoms when compressed by destroyed intervertebral discs.

The signs of neck osteochondrosis depend on which body system is affected by the pathology: Below we consider the general clinic of osteochondrosis of the cervical spine.
Pain in the back of the head, neck and collar area
This is the most common symptom. The pain location can be widespread and affect the shoulders, collarbone area and chest, which can lead to severe migraine headaches.
The nature of the pain depends on the location of the lesion and the severity of the pathology. In the first stages of disease development, pain can quickly be temporary and gradually become chronic and painful.
During exacerbations, the pain becomes stabbing, with increased tone of the neck muscles and limited head movement. Often, pain in cervical osteochondrosis can be localized behind the sternum, which is why many patients confuse this symptom with angina pectoris. Differentiation can be done by taking a nitroglycerin tablet - this does not relieve pain from osteochondrosis.

Noise, ringing, feeling of fullness in the ears
These symptoms are often accompanied by hearing loss. These phenomena are associated with a decrease in blood flow from the vertebral arteries to the vestibular apparatus. The complex of these symptoms is called cochlear or cochlear syndrome and it is not always possible to determine its connection with osteochondrosis in the neck region. A specific distinguishing feature is that when changing position, after staying in one position for a long time, noises, congestion and ringing in the ears can be felt.
dizziness
Dizziness is also caused by impaired blood flow to the organs of the inner ear, which ensure the balance of the body. Dizziness is often accompanied by nystagmus - arbitrary fluctuations of the eye pupils to the side.
Lack of air
This feeling occurs due to irritation of the ends of the phrenic nerve. It is part of the cervical nerve bundle and is involved in the regulation of breathing, its depth and frequency. Patients complain of the inability to breathe deeply. In some cases, the symptom worsens to severe shortness of breath and suffocation. For the same reason, pauses in breathing and snoring occur at night. Lack of oxygen due to breathing problems ultimately leads to increased fatigue, reduced concentration and memory problems.
nausea
Accompanied by belching of air. It is also caused by poor circulation in certain areas of the brain and inner ear. Sometimes nausea is observed with uncontrollable vomiting caused by movements of the head and body. Frequent nausea and vomiting lead to decreased appetite, weight loss, and nutrient deficiencies.
Visibility problems
"Swimming" in the eyes, reduced visual acuity, fog in front of the eyes – all these are symptoms caused by ischemia of the part of the brain responsible for vision. Patients with osteochondrosis are less likely to complain about visual impairment due to insufficient blood supply from the vertebral vesselsis balanced by blood flow from the carotid system. Glasses and therapeutic exercises for the eye muscles do not solve the problem; as a rule, vision improves after osteochondrosis treatment.
Blood pressure rises
Unstable pressure levels are caused by impaired blood circulation in the medulla oblongata, which is responsible for the functions of the vascular-motor center.
Sudden fainting or syncope
Occurs when the cerebral arteries spasm due to a momentary interruption of blood flow through the vertebral arteries. The patient can be quickly brought out of the state of unconsciousness by lying him down so that his legs are slightly higher than his head - blood flow to the brain allows the person to be brought back to consciousness. After a fainting attack, reversible speech and movement disorders can occur for some time due to a brief stop in blood flow.
Throat symptoms
Often they can be the only sign of cervical osteochondrosis. Externally as pain, dryness and a lumpy feeling in the throat, difficulty swallowing. The symptoms are accompanied by compression of the nerve plexuses that are responsible for the innervation of the throat. It is necessary to distinguish such manifestations from a similar clinic with inflammation or neoplasms.
Increase in body temperature
An increase in body temperature with cervical osteochondrosis is not the most typical symptom; It is observed rarely and locally: in the neck and collar area with slight reddening of the skin. The clinic of osteochondrosis in the cervical spine can, firstly, be of different degrees of severity, it depends on the stage of development of the pathologies, even in periods of exacerbations they are brighter, and secondly, they develop into certain syndromes.
Symptoms depend on the stage of cervical osteochondrosis
Stage I: Beginning of degenerative processes in the cartilage of the intervertebral discs. Symptoms are mild and sometimes not observed at all. Important: These symptoms increase when the head is tilted.
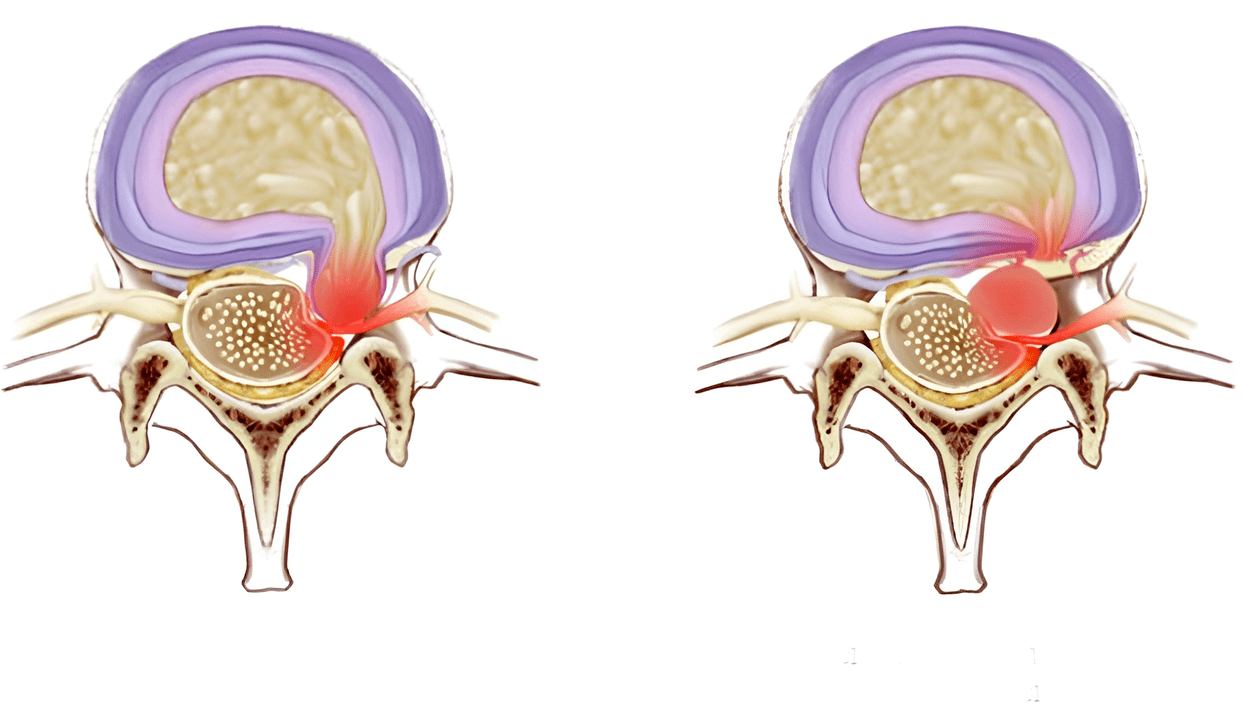
In the first stage of cervical osteochondrosis, patients usually do not go to the doctor, believing that all symptoms are associated with fatigue, stress, age and lack of sleep. Stage II In this stage, the protrusion of the intervertebral discs has begun, the intervertebral spaces narrow and the collagen fiber of the fibrous ring of the intervertebral disc is destroyed. Due to the compression of the nerve trunks, noticeable pain symptoms of a punctual nature occur, which intensify when the neck is moved and the head is turned. Cervical osteochondrosis can already be suspected here, the symptoms of which in the second stage look as follows: 1. , 2. , 3. and 4.
Holding your head in one position for a long time causes severe pain. At this stage of the disease, patients already turn to the doctor. Stage III The fibrous ring in the intervertebral disc is destroyed and hernias form. In the third stage, due to their weak fixation, spinal deformations, displacements and dislocations of the vertebrae are observed.
This is a serious stage of the disease in which the patient can no longer support their head independently. Ischemia of the spinal cord and compression of the spinal arteries lead to paralysis and paresis in other parts of the body and spinal stroke.
Syndromes caused by osteochondrosis of the cervical spine
The nonspecificity and variety of different symptoms associated with cervical osteochondrosis complicate diagnosis and further treatment, since some of them can be a sign of completely different diseases. The symptoms of cervical osteochondrosis can be divided into specific groups called syndromes. Their presence and severity may indicate pathology of the cervical spine with a specific localization.
A group of common syndromes:
Koreshkovy. Also called cervical radiculitis. It combines symptoms associated with pinched nerve roots of the cervical vertebrae. Characterized by "goosebumps" in the affected area, tingling in the fingers and forearms, and doughy skin spreading to certain fingers.
Irritating-reflexive. Burning and acute pain in the back of the head and neck, sometimes radiating to the chest and shoulder, and occurring when the position of the head and neck changes when sneezing, coughing, or turning the head sharply.
Vertebral artery syndrome includes:
Heart. An almost identical picture in angina pectoris often leads to incorrect diagnosis and treatment. The syndrome occurs due to irritation of the receptors of the phrenic nerve, partially affecting the pericardium and pectoralis major muscle. Cramps in the heart area are therefore more of a reflex in response to irritation of the cervical nerves. Symptoms:
Vegetative-dystonic syndrome. Subluxation of the first cervical vertebra with displacement can lead to the development of vegetative-vascular dystonia. VSD is not a clear diagnosis because it does not have pronounced symptoms.
Neurological symptoms, symptoms of impaired cerebral circulation, an increase in intracranial pressure and muscle spasms may occur. As a result, the patient's complaints boil down to dizziness, reduced visual acuity, loss of consciousness, headache and nausea.
How to treat cervical osteochondrosis?
The described condition of the spine is a very serious pathology, which, if ignored, leads to disability and, as a result of serious disorders of cerebral circulation, death. For this reason, you should not self-medicate if such symptoms occur.
At the initial stage, treatment of cervical osteochondrosis is conservative and includes medications: non-steroidal anti-inflammatory drugs, anesthetics, hormones, vitamin complexes, chondroprotectors - all this relieves inflammation, pain and improves the trophism of soft tissues and cartilage vertebrae.







































